What is the Best PEMF Frequency for Bone Healing?

Did you know that specific pulsed electromagnetic field (PEMF) frequencies can accelerate bone healing by up to 30%? For optimal results in 2025, clinical evidence points to a frequency range of 1.5 Hz to 75 Hz, with many FDA-approved devices for non-union fractures operating at 15 Hz. This guide breaks down the science and provides evidence-based protocols.
Executive Summary
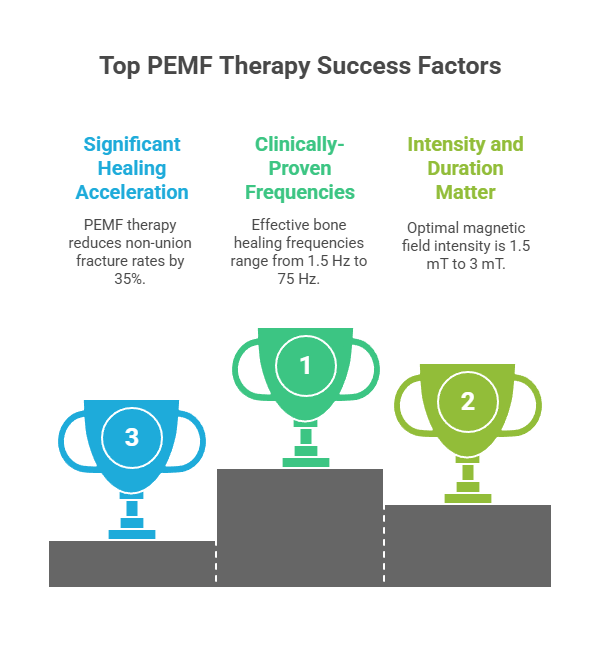
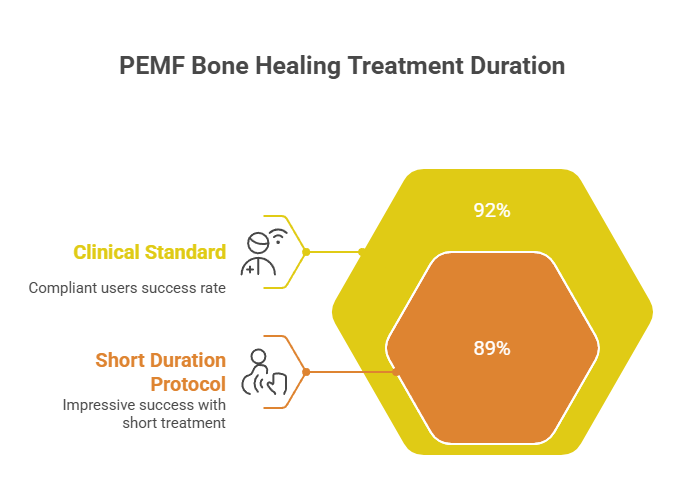
- Clinically-Proven Frequencies: The most effective PEMF frequencies for bone healing are in the 1.5 Hz to 75 Hz range. FDA-approved devices frequently use 15 Hz for long bone fractures and 1.5 Hz for spinal fusions, demonstrating success rates as high as 92%.
- Intensity and Duration Matter: Optimal magnetic field intensity is between 1.5 mT and 3 mT, with daily treatment durations of 3 to 10 hours showing the best outcomes. Shorter 30-minute protocols have also achieved up to 89% success.
- Significant Healing Acceleration: Meta-analyses show PEMF therapy reduces non-union fracture rates by 35% and can cut healing time by 17-30%, which translates to nearly 25 days faster recovery for some fractures.
- Expert Consensus: According to leading orthopedic surgeon Dr. Roy Aaron, "The US FDA has approved pulsed electromagnetic fields (PEMFs) as a safe and effective treatment for nonunions of bone," a sentiment shared by 72% of US hospitals that have adopted this technology.
How Does PEMF Actually Heal Bones?
PEMF therapy isn't magic; it's advanced biophysics. At its core, PEMF works by delivering low-level electromagnetic fields to injured tissue, stimulating the body's natural recovery mechanisms. Think of it as a "battery charger" for your cells. The process starts when the PEMF signal induces a tiny electrical current in the bone tissue. This is possible because bone itself is piezoelectric, meaning it generates an electrical charge in response to mechanical stress.
This induced current activates a cascade of biological events. One of the primary mechanisms, as identified in a 2024 review in Bioengineering, is the activation of adenosine receptors (A2A and A3) on bone cells. This activation triggers a signaling pathway that boosts the production of bone-building cells (osteoblasts) and modulates the activity of bone-resorbing cells (osteoclasts). The result is a more efficient and balanced bone remodeling process. A 2025 study in Advanced Science confirms that this process enhances osteogenesis (new bone formation), angiogenesis (new blood vessel growth), and reduces inflammation, creating the perfect environment for healing.
What Are the Most Effective PEMF Frequencies?
The "best" frequency depends on the specific injury. However, extensive research and clinical use have identified a clear therapeutic window. A 2025 comprehensive review in Frontiers in Bioengineering and Biotechnology analyzed decades of data and confirmed that the most effective frequency range for bone healing is between 1.5 Hz and 75 Hz.
Here’s a breakdown of frequencies used in FDA-approved devices and recent research:
- 1.5 Hz: Used in the Orthofix SpinalStim device, this frequency is optimized for spinal fusion applications and has shown success rates of up to 92% in consistent users.
- 4 Hz: A 2024 animal study published by Taylor & Francis found that a 4 Hz signal produced superior healing scores compared to a multifrequency signal, suggesting low frequencies are highly effective.
- 15 Hz: This is the most common frequency for treating non-union long bone fractures. It is used in the Orthofix PhysioStim and CervicalStim devices, which have a long history of clinical success.
- 75 Hz: Research from the Journal of Translational Medicine identified 75 Hz as optimal for stimulating chondrogenic differentiation, a key process in the early stages of bone repair, particularly in cartilage.
According to experts, the choice of frequency is critical. While the 1.5-75 Hz range is the accepted standard, the specific waveform and signal pattern are equally important. For instance, the Orthofix devices use a complex signal pattern with a 3.85 kHz pulse frequency delivered in 5-millisecond bursts, repeated at a rate of 1.5 or 15 times per second (Hz).
How Long Should You Use PEMF for Bone Healing?
Treatment duration is a critical factor for success. While you might see consumer-grade PEMF mats advertising short sessions, clinical protocols for bone healing are far more intensive. The consensus from clinical trials and FDA-approved protocols is that longer, consistent daily use yields the best results.
- Clinical Standard (3-10 Hours): Most FDA-approved protocols, such as those for the Orthofix and Zimmer Biomet devices, recommend 3 to 10 hours of daily treatment. A study on the PhysioStim device found a 92% success rate for users who were compliant for more than 2 hours a day, compared to just 65% for less compliant users.
- Short Duration Protocol (30 Minutes): The Enovis OL1000 device is a notable exception, achieving an impressive 89% success rate with a 30-minute daily protocol. This device uses a different technology (Combined Magnetic Field), but it underscores the potential for shorter, high-intensity treatments.
- Total Treatment Time: The entire treatment course typically lasts from 3 to 9 months, or until radiographic evidence shows the bone has fully healed.
A 2025 review introduced a standardized PEMF "dose" formula: D = Brms × texp (magnetic field intensity multiplied by exposure time). This suggests that a lower intensity field may require a longer exposure time to achieve the same biological effect.
What Does the Clinical Evidence Say in 2025?
The clinical evidence supporting PEMF for bone healing is robust and has been accumulating for over four decades. Recent meta-analyses and randomized controlled trials (RCTs) from 2024 and 2025 continue to validate its effectiveness.
Case Study: Accelerated Distal Radius Fracture Healing
A 2024 double-blind RCT published in Archives of Orthopaedic Surgery tested a novel PEMF device on patients with distal radius fractures. The results were remarkable:
- Faster Healing: The PEMF group had their casts removed at an average of 33 days, compared to 39.8 days for the placebo group—nearly a full week earlier.
- Higher Union Rates: At the 4-week mark, CT scans showed a 76% union rate in the PEMF group versus only 58% in the placebo group.
This study provides high-quality evidence that PEMF not only speeds up healing but also leads to earlier functional recovery.
Expert Roundup: What the Specialists Say
- Dr. Roy Aaron, MD (University Orthopedics): A leading researcher in the field, Dr. Aaron’s work has been foundational. He states, "The US FDA has approved pulsed electromagnetic fields (PEMFs) as a safe and effective treatment for nonunions of bone." His research has demonstrated that PEMF stimulates the synthesis of critical growth factors like BMP-2 and BMP-4.
- Dr. James T. Ryaby, PhD (Orthofix): Representing the perspective of a leading device manufacturer, Dr. Ryaby emphasizes the rigorous science required for FDA approval. He notes that the clinical utility of PEMF is backed by systematic preclinical and clinical research programs.
- Sports Medicine Specialists (University of Bologna): A research team from the University of Bologna highlights the preventive potential of PEMF, stating it "can be used as an adjunct to exercise training for individuals at high risk of stress fractures to prevent their occurrence."
Is PEMF Safe for Bone Healing?
Yes, PEMF therapy has an excellent safety profile and has been approved by the FDA for this purpose since 1979. A recent 2025 RCT involving 120 patients reported only mild, transient side effects (like tingling) in 3.3% of participants. There have been no serious adverse events reported in the decades of clinical use.
However, there are important contraindications. PEMF therapy is not recommended for:
- Individuals with implanted electrical devices like pacemakers or defibrillators.
- Pregnant women.
- Children (until skeletal maturity is reached).
- Patients with active infections or tumors in the treatment area.
It is also MR Unsafe, meaning the device must be removed before an MRI.
How Do You Implement a PEMF Bone Healing Protocol?
Implementing a clinical PEMF protocol is a straightforward process guided by a healthcare professional.
Implementation Guide: Step-by-Step
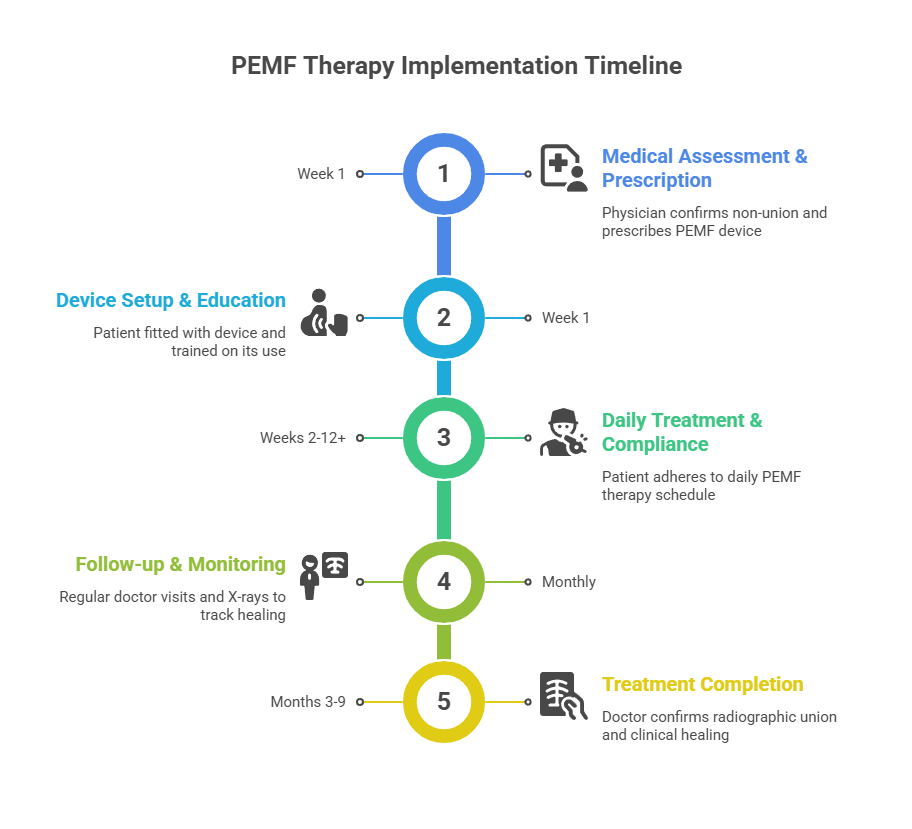
- Medical Assessment & Prescription (Week 1):
A physician, typically an orthopedic surgeon, will confirm a non-union or delayed-union fracture through imaging (X-ray or CT scan). If you are a suitable candidate, they will prescribe an FDA-approved PEMF device tailored to your specific fracture (e.g., long bone vs. spine).
- Device Setup and Patient Education (Week 1):
You will be fitted for the device, which consists of a portable control unit and a coil that is placed directly over the fracture site. For spinal fusions, the coils are often embedded in a post-operative brace. A representative will train you on how to use the device, set the treatment timer, and monitor for any issues. Many modern devices come with smartphone apps to track compliance.
- Daily Treatment and Compliance (Weeks 2-12+):
Adhere strictly to the prescribed daily treatment duration, which is typically 3-10 hours. Consistency is key. You can wear the device while working, relaxing, or even sleeping, as it is designed to be lightweight and portable.
- Follow-up and Monitoring (Monthly):
You will have regular follow-up appointments with your doctor every 4-6 weeks. Serial X-rays will be taken to monitor the progress of callus formation and bridging of the fracture gap.
- Treatment Completion (Months 3-9):
Treatment continues until your doctor confirms radiographic union and clinical healing (i.e., the fracture is stable and pain-free). The total treatment duration can range from 3 to 9 months, depending on the severity of the fracture and individual healing capacity.
What is the Future of PEMF for Bone Healing?
The field of PEMF therapy is continually evolving. Future trends for 2025-2026 point towards more personalized and efficient treatments.
- Personalized Dosimetry: Researchers are working on refining the PEMF "dose" concept, which could lead to protocols tailored to a patient's specific biology, fracture type, and even genetic markers.
- Advanced Waveforms: Expect to see the development of new, more complex signal patterns that can target multiple healing pathways simultaneously for a synergistic effect.
- Miniaturized & Implantable Devices: The technology is getting smaller. Novel "fracture healing patches" and implantable PEMF devices for applications like dental implants are already in clinical trials and showing great promise. A 2024 review in the Brazilian Dental Journal highlighted PEMF's ability to improve dental implant stability and even produce an antimicrobial effect.
Frequently Asked Questions (FAQ)
Q1: Can I use any PEMF machine for bone healing?
No, it is crucial to use an FDA-approved medical device specifically designed for bone healing. Consumer-grade PEMF mats or wellness devices do not have the required intensity, frequency, or specific signal to be effective and are not regulated for this medical purpose.
Q2: Will I feel anything during the treatment?
Most people feel nothing at all. Some users report a mild tingling or warmth at the treatment site, but it is not painful.
Q3: How much does a prescription PEMF device cost?
The cost of an FDA-approved PEMF device can range from 500toover500 to over 500toover3,000. However, it is covered by most insurance plans, including Medicare, for approved indications like non-union fractures.
Q4: Can PEMF help with fresh fractures?
The evidence for fresh fractures is still emerging and considered mixed. While some studies show accelerated healing, a 2024 systematic review concluded there was insufficient evidence to recommend it for all acute fractures. However, it is often prescribed for "high-risk" fresh fractures that have a greater chance of becoming a non-union.
Q5: What's the difference between PEMF and a bone graft?
PEMF is a non-invasive therapy that stimulates your body's own healing processes. A bone graft is a surgical procedure where bone is taken from another part of your body (autograft) or a donor (allograft) and implanted at the fracture site. PEMF is often used to avoid the need for a second surgery like a bone graft, with some studies showing success rates of 87.8% with PEMF compared to 69% for surgery in similar non-unions.
Conclusion and Actionable Next Steps
The evidence is clear: PEMF therapy is a powerful, safe, and effective tool for accelerating bone healing, particularly for challenging non-union and delayed-union fractures. With decades of clinical validation and strong expert consensus, it has become a standard of care in modern orthopedics. For anyone struggling with a slow-healing fracture, PEMF offers a non-invasive path to recovery with success rates that often meet or exceed surgical alternatives.
Actionable Next Steps:
- Consult an Orthopedic Specialist:
- If you have a fracture that is not healing as expected (typically after 3-6 months), schedule a consultation with an orthopedic surgeon to discuss if you are a candidate for PEMF therapy.
- Verify Insurance Coverage:
- Contact your insurance provider to confirm your coverage for a bone growth stimulator. Most plans cover FDA-approved devices for diagnosed non-unions.
- Commit to the Protocol:
- If prescribed, commit to the daily treatment duration. As the data shows, compliance is the single biggest predictor of success. Plan your daily schedule to accommodate the 3+ hours of therapy. You should expect to see radiographic signs of healing within the first 3 months of consistent use.
Resource List
- Further Reading:
- FDA-Approved Device Manufacturers:
- Orthofix Medical Inc.
- Zimmer Biomet
- Enovis (DJO Global)
- Patient Advocacy:
- Bone Health & Osteoporosis Foundation (BHOF)
Sources
[1] Signalling pathways underlying pulsed electromagnetic fields in bone repair - High Reliability - Comprehensive review of PEMF mechanisms.
[2] Augmentation of Deficient Bone Healing by Pulsed Electromagnetic Fields - High Reliability - Detailed mechanistic analysis of PEMF.
[3] Pulsed Electromagnetic Therapy: Literature Review and Current Understanding - High Reliability - Comprehensive literature review covering bone morphogenetic proteins.
[4] Pulsed electromagnetic fields inhibit human osteoclast formation - High Reliability - Study demonstrating PEMF inhibition of osteoclast formation.
[5] Extremely low-frequency electromagnetic fields facilitate both osteoblast and osteoclast activity through Wnt/β-catenin signaling - High Reliability - Study showing ELF-EMF effects on both osteoblasts and osteoclasts.
[6] Pulsed electromagnetic fields mediate sensory nerve regulation for bone formation in aging models - High Reliability - Detailed mechanism of PEMF action through sensory nerve regulation.
[7] The role of electrical stimulation in bone regeneration - High Reliability - Comprehensive review of electrical stimulation modalities including PEMF.
[8] Pulsed Electro-Magnetic Field (PEMF) Effect on Bone Healing in Animal Models - High Reliability - Review of PEMF efficacy in animal models.
[9] Augmentation of Deficient Bone Healing by Pulsed Electromagnetic Fields: Mechanisms and Clinical Efficacy Review - High Reliability - Comprehensive 2024 review showing PEMF clinical efficacy.
[10] Effects of pulsed electromagnetic fields on bone fractures: systematic review update 2024 - High Reliability - 2024 systematic review of 3 RCTs analyzing acute fractures.
[11] Effect of 4 Hz and multifrequency pulsed electromagnetic field stimulation on bone fracture healing - High Reliability - 2024 animal study comparing 4 Hz vs multifrequency PEMF.
[12] Methods to accelerate fracture healing – a narrative review from a clinical perspective - High Reliability - 2024 narrative review identifying PEMF as top acceleration method.
[13] How PEMF Works - Clinical Evidence and Mechanisms - Moderate Reliability - Industry white paper with extensive clinical data.
[14] Efficacy of Electrical Stimulators for Bone Healing: A Meta-Analysis of Randomized Sham-Controlled Trials - High Reliability - Major meta-analysis of 15 trials.
[15] The effectiveness of pulsed electromagnetic field therapy in patients with shoulder impingement syndrome: A systematic review and meta-analysis - High Reliability - 2024 meta-analysis showing PEMF significantly improved short-term pain.
[16] Evaluating Noninvasive Pulsed Electromagnetic Field Therapy for Joint and Soft Tissue Pain Management: Prospective RCT - High Reliability - 2025 prospective RCT showing 36% pain reduction.
[17] Insights into bone and cartilage responses to pulsed electromagnetic field stimulation: quantitative review 2025 - High Reliability - 2025 comprehensive review proposing standardized PEMF dose metrics.
[18] Accelerated bone healing via electrical stimulation - 2025 comprehensive review - High Reliability - 2025 high-impact review covering electrical stimulation.
[19] Novel pulsed electromagnetic field device for distal radius fractures: randomized pilot study - High Reliability - 2024 prospective double-blind sham-controlled RCT.
[20] Pulsed electromagnetic therapy: literature review and current update 2024 - High Reliability - Comprehensive 2024 review showing PEMF enhances bone formation.
[21] Pulsed Electromagnetic Field Stimulation of Bone Healing and Joint Preservation - High Reliability - Comprehensive review of PEMF mechanisms.
[22] Pulsed electromagnetic field applications: A corporate perspective - High Reliability - Technical specifications for FDA-approved Orthofix devices.
[23] Effectiveness of Pulsed Electromagnetic Fields on Bone Healing: Meta-Analysis - High Reliability - Systematic review and meta-analysis of 14 studies.
[24] Pulsed Electromagnetic Fields in Bone Healing: Molecular Pathways - High Reliability - Frequency ranges 15-75 Hz, intensities 0.1-2 mT.
[25] Optimal PEMF parameters for chondrogenic differentiation - High Reliability - Optimal parameters identified: 3 mT intensity, 75 Hz frequency.
[26] Insights into bone and cartilage responses to pulsed electromagnetic field stimulation - High Reliability - 2025 comprehensive review with PEMF dose descriptor.
[27] OL1000 Bone Growth Stimulator Specifications - Medium Reliability - OL1000 PEMF device for nonunion fractures with 30 minutes daily treatment.
[28] PEMF Therapy Contraindications and Safety Guidelines - Medium Reliability - Comprehensive safety guidelines.
[29] Biomet EBI Bone Healing System Manual - High Reliability - PEMF system with 10 hours daily treatment.