Prostate Problems Erectile Disfunction
If you're one of the millions of men dealing with an enlarged prostate (benign prostatic hyperplasia or BPH), you know how frustrating the symptoms can be. Frequent nighttime bathroom trips, a weak urinary stream, and the constant feeling that your bladder isn't fully empty can significantly impact your quality of life.
The traditional medical route often presents you with two less-than-ideal options: lifelong medications with unwanted side effects, or invasive surgery with its own risks and recovery challenges. But what if there was a third option—a non-surgical, drug-free treatment that could potentially reduce your prostate size and relieve symptoms?
Pulsed electromagnetic field (PEMF) therapy is emerging as a promising non-invasive treatment option for enlarged prostate. Recent pilot studies have shown encouraging results, with men experiencing symptom relief and measurable prostate shrinkage—all without surgery or pharmaceuticals. However, it's important to note that this research is still in early stages, and larger clinical trials are needed to fully establish efficacy.
In this comprehensive guide, we'll explore how PEMF therapy works, compare it to traditional treatments, and show you what current research says about this developing technology and how it might help you reclaim your comfort and confidence.
Understanding Enlarged Prostate (BPH): More Than Just a Nuisance
What Is Benign Prostatic Hyperplasia?
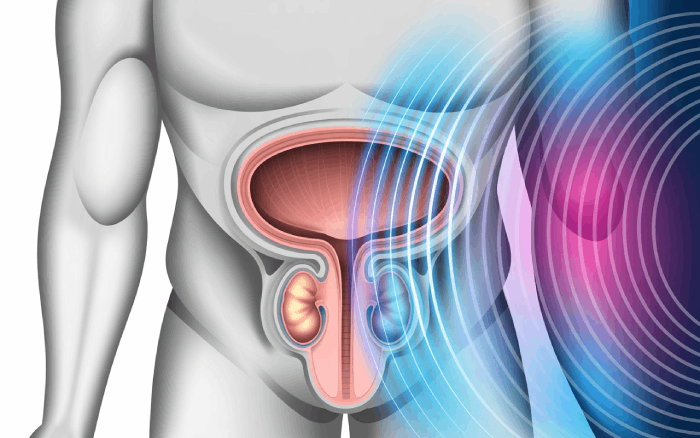
Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland that affects approximately 50% of men over age 50 and up to 90% of men over age 80.[1,2] As the prostate enlarges, it wraps around the urethra (the tube that carries urine from the bladder), gradually squeezing it and restricting urine flow.
BPH is a histologic diagnosis describing the proliferation of smooth muscle and epithelial cells within the prostatic transition zone. The prevalence and severity of lower urinary tract symptoms (LUTS) in aging men are progressive and can significantly impact quality of life.[3]
Common BPH Symptoms That Disrupt Daily Life
Men with an enlarged prostate typically experience:
Urinary Symptoms:
- Frequent urination (especially at night - nocturia)
- Sudden, urgent need to urinate
- Weak or slow urinary stream
- Difficulty starting urination
- Dribbling at the end of urination
- Inability to completely empty the bladder
- Intermittent stream (stopping and starting)
Impact on Quality of Life:
- Sleep disruption from multiple nighttime bathroom trips
- Anxiety about being near a bathroom
- Reduced social activities and travel
- Embarrassment and frustration
- Sexual dysfunction in some cases
Why BPH Happens
While the exact cause isn't fully understood, BPH is associated with several factors:
- Hormonal changes with aging - Increased dihydrotestosterone (DHT) and altered androgen/estrogen balance
- Chronic low-grade inflammation - Research shows 43-98% of BPH tissues contain inflammatory infiltration[4,5]
- Changes in cell growth and death balance - Disrupted cellular homeostasis
- Reduced blood flow to prostate tissue and tissue hypoxia[6]
- Stromal-epithelial interactions - Growth factors and cytokines promote cell proliferation[7]
The key factor emphasized in recent research? Chronic inflammation plays a major role in BPH pathogenesis—and this is where PEMF therapy may be beneficial.[4,5,8]
Traditional BPH Treatment Options: The Current Landscape
Before we dive into PEMF therapy, let's examine what most men face when diagnosed with BPH, according to current American Urological Association (AUA) guidelines.[9,10]
Option 1: Medications
Alpha-Blockers (Flomax, Uroxatral, Rapaflo):
- How they work: Relax prostate and bladder muscles to address the dynamic component of BPH
- Timeline: Symptom relief in 1-2 weeks, with maximum effect at 72 hours
- Typical improvement: 4-6 points on symptom scores
- Downsides: Dizziness, fatigue, retrograde ejaculation, intraoperative floppy iris syndrome (IFIS) for cataract surgery, lifelong use required
- Cost: $50-$200/month ongoing
5-Alpha Reductase Inhibitors (Finasteride, Dutasteride):
- How they work: Shrink prostate by blocking DHT hormone production
- Timeline: 6-12 months for full effect; prostate volume reduction of 20-30%
- Downsides: Sexual side effects (ED, decreased libido), requires 6+ months to see benefits
- Cost: $30-$150/month ongoing
Combination Therapy:
- Uses both drug types together for moderate-to-severe symptoms with prostatic enlargement
- More effective for symptom reduction and preventing progression
- Compounds side effects
- Most expensive medication option[9]
Option 2: Minimally Invasive Procedures
UroLift:
- Small implants hold prostate tissue away from urethra
- Office-based procedure
- Cost: $5,000-$8,000
- Preserves sexual function but may need repeat procedures
Rezūm Water Vapor Therapy:
- Steam destroys excess prostate tissue
- Office-based, quick recovery
- Cost: $3,000-$5,000
- Good results but tissue destruction is irreversible
Prostatic Artery Embolization (PAE):
- Blocks blood flow to prostate
- Hospital-based procedure
- Cost: $10,000-$15,000
- AUA notes unclear benefit-to-risk ratio; recommended only in select patients and clinical trials[9]
Option 3: Surgical Treatments
TURP (Transurethral Resection of Prostate):
- "Gold standard" surgery - removes prostate tissue
- Requires general anesthesia and hospital stay
- Cost: $10,000-$20,000
- Risks: Bleeding, infection, sexual dysfunction (including ejaculatory dysfunction), incontinence
- Recovery: 4-6 weeks
Laser Surgery (Greenlight PVP, HoLEP, ThuLEP):
- Laser vaporizes or enucleates excess tissue
- Less bleeding than TURP; effective for larger prostates
- Cost: $8,000-$15,000
- Similar risks to TURP including ejaculatory dysfunction[10]
The Problem With Traditional Options
While these treatments can be effective, they all have significant considerations:
- Medications: Lifelong commitment, side effects, don't address root inflammatory cause
- Procedures: Invasive, expensive, risk of complications
- Surgery: Most invasive, longest recovery, highest risk of side effects
This is why men are increasingly seeking non-invasive alternatives that may address the underlying inflammation rather than just managing symptoms or destroying tissue.
PEMF Therapy: An Emerging Non-Surgical BPH Treatment
What Is PEMF Therapy?
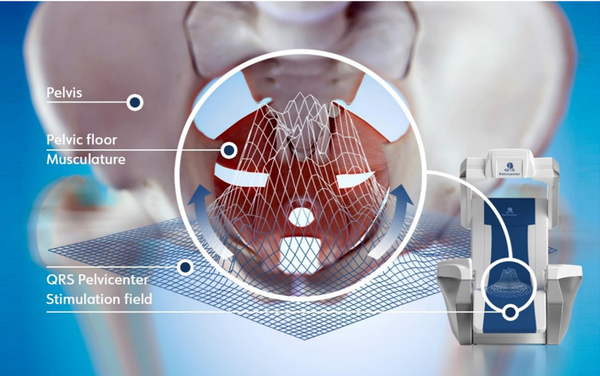
Pulsed electromagnetic field (PEMF) therapy uses low-frequency electromagnetic waves (typically 1-50 Hz) to stimulate cellular repair and reduce inflammation throughout the body.[11] When applied to the prostate region, these electromagnetic pulses penetrate deep into tissues to potentially promote healing at the cellular level.
Think of PEMF as a "cellular tune-up" that may help your body's natural healing mechanisms work more efficiently.
How PEMF Works on Enlarged Prostate (Proposed Mechanisms)
Research suggests PEMF therapy may address BPH through multiple mechanisms:[11,12]
1. Reduces Chronic Inflammation
BPH is driven largely by chronic low-grade inflammation in prostate tissue.[4,5,8] PEMF therapy may:
- Decrease pro-inflammatory cytokines (IL-2, IL-4, IL-8, IL-17, IFN-γ) and growth factors (VEGF, TGF-β, FGF-2)
- Reduce tissue swelling around the urethra
- Create an environment more conducive to healing
2. Improves Blood Circulation
Electromagnetic pulses may stimulate vasodilation (blood vessel widening), which could:
- Deliver more oxygen and nutrients to prostate cells
- Remove metabolic waste products more efficiently
- Reduce tissue hypoxia, which is implicated in BPH progression[6,12]
3. Promotes Cellular Repair
PEMF may enhance cellular energy production by:
- Increasing intracellular calcium (Ca2+) binding to calmodulin
- Activating endothelial nitric oxide synthase (eNOS)
- Boosting nitric oxide (NO) synthesis from L-arginine
- Supporting tissue regeneration and remodeling[11]
4. Reduces Tissue Hypoxia
The overall effect is a potential reduction in tissue hypoxia and therefore a reduction in prostatic growth driven by the inflammation-fibrosis-hypoxia cycle.[11,13]
5. Reduces Prostate Volume
The combination of reduced inflammation, improved circulation, and cellular optimization may lead to:
- Measurable shrinkage of prostate tissue
- Relief of pressure on the urethra
- Improved urinary flow
Watch: How PEMF Therapy Works for Enlarged Prostate
In this video, we demonstrate the PEMF therapy process and explain the science behind how it reduces prostate enlargement.
Clinical Evidence: Does PEMF Really Work for BPH?
The Landmark 28-Day Human Study
A pilot study published in Andrology by researchers at Sapienza University of Rome evaluated PEMF therapy for 27 men with benign prostatic hyperplasia.[11] The results were encouraging:
Study Design:
- 27 treatment-naive patients with BPH and LUTS
- Used handheld PEMF device (Magcell® Microcirc, Physiomed Elektromedizin)
- Treatment: 5 minutes twice daily for 28 consecutive days
- Measurements: Transrectal ultrasound, IPSS scores, IIEF-15, hormone levels
Study Results:
- Prostate volume reduction: Median decrease of 5.4% after just 28 days
- Symptom improvement: Significant reduction in lower urinary tract symptoms (LUTS) measured by IPSS
- Speed of results: Benefits appeared within 3-4 weeks
- Safety profile: No serious adverse effects reported; high compliance
- Hormone levels: No negative impact on testosterone or sexual function
- Duration: Effects were maintained at 4-month follow-up
Important Context:
- Patients with moderate-severe LUTS and without metabolic syndrome benefited more from treatment
- This was a pilot study with a small sample size (27 patients)
- No control group was included
- Larger randomized controlled trials are needed to confirm these findings[11,14]
The Canine Model Study
Prior to the human study, researchers conducted a pilot study in 20 dogs with naturally occurring BPH.[12] Results were dramatic:
- Average 57% reduction in prostatic volume following 3 weeks of treatment (5 minutes, twice daily)
- No interference with semen quality, testosterone levels, or libido
- Significant reduction in peripheral vascular resistances
- Progressive reduction in blood flow velocity in prostatic artery
- Confirmed safety with no side effects
Why the difference between dogs and humans? The larger reduction in dogs may be due to differences in prostate tissue architecture and growth characteristics between species.[11,14] Human prostates have a more complex structure with both glandular and stromal components.
Previous Studies
Two earlier published studies used desktop PEMF devices to treat BPH in men with positive but variable results, though these studies had methodological limitations.[15,16]
What Makes These Results Significant?
While a 5.4% reduction might sound modest, consider that:
- Results appeared in less than one month (vs. 6-12 months for 5-ARIs)
- The treatment was completely non-invasive
- No side effects on sexual function were reported
- Symptoms improved substantially
- This was achieved with a portable, patient-administered device
- The effect was maintained over several months
However, it's crucial to emphasize: These are preliminary findings from small pilot studies. Much larger randomized controlled trials with control groups are needed before PEMF can be considered an established treatment for BPH.[11,14]
PEMF vs. Traditional BPH Treatments: A Direct Comparison
Here's how PEMF therapy stacks up against conventional options based on current evidence:
| Treatment | Invasiveness | Results Timeline | Prostate Shrinkage | Side Effects | Cost | Sexual Function | Evidence Level |
|---|---|---|---|---|---|---|---|
| PEMF Therapy | Non-invasive | 3-4 weeks | Limited data (5.4% in pilot study) | Minimal/none | $500-$6,000 (device) | No impact | Preliminary (small pilots) |
| Alpha-Blockers | Non-invasive | 1-2 weeks | No | Dizziness, fatigue, sexual | $600-$2,400/year | May cause issues | Strong evidence |
| 5-ARIs | Non-invasive | 6-12 months | Yes (20-30% reduction) | ED, low libido | $360-$1,800/year | Often impaired | Strong evidence |
| Combination Therapy | Non-invasive | 2-4 weeks/6-12 months | Yes | Combined side effects | $1,000-$4,000/year | May be impaired | Strong evidence |
| UroLift | Minimally invasive | Immediate | No | Pain, urgency | $5,000-$8,000 | Generally preserved | Moderate evidence |
| Rezūm | Minimally invasive | 2-4 weeks | Yes (tissue destruction) | Temporary urgency | $3,000-$5,000 | Generally preserved | Moderate evidence |
| TURP Surgery | Invasive | Immediate | Yes (removal) | Bleeding, infection, EjD | $10,000-$20,000 | Often impaired | Strong evidence |
| Laser Surgery | Invasive | Immediate | Yes (vaporization) | Bleeding, infection, EjD | $8,000-$15,000 | Often impaired | Strong evidence |
EjD = Ejaculatory dysfunction
Why Consider PEMF Therapy?
Potential Advantages:
- ✅ Completely non-invasive (no anesthesia, no incisions)
- ✅ No systemic side effects like medications
- ✅ May address root cause (inflammation) rather than just symptoms
- ✅ Preserves all tissue and function
- ✅ Can be done at home with appropriate devices
- ✅ One-time investment for long-term use
- ✅ No reported impact on sexual function
- ✅ Safe for long-term use in preliminary studies
- ✅ Can potentially be combined with other therapies if needed
Important Limitations:
- ⚠️ Evidence is preliminary - only small pilot studies published
- ⚠️ No large randomized controlled trials yet
- ⚠️ Long-term efficacy beyond 4 months unclear
- ⚠️ Not included in AUA guidelines as standard treatment
- ⚠️ May not be sufficient for severe BPH or complications
Best Suited For:
- Men with mild to moderate BPH who want to explore emerging options
- Those who want to avoid surgery or are poor surgical candidates
- Men experiencing medication side effects
- Patients seeking complementary approaches alongside conventional care
- Those with concerns about sexual function
- Men willing to commit to daily treatment protocol
- Those understanding this is investigational with limited evidence
How PEMF May Relieve Specific BPH Symptoms
Let's break down exactly how PEMF therapy might address each frustrating symptom of an enlarged prostate, based on proposed mechanisms:
Urinary Frequency and Urgency
The Problem: Prostate inflammation irritates the bladder, creating false signals of fullness.
How PEMF May Help:
- Potentially reduces inflammation around bladder neck
- May calm overactive nerve signals
- Could normalize bladder sensitivity
- Potential Result: Fewer urgent trips, especially at night
Weak Urinary Stream
The Problem: Enlarged prostate tissue physically constricts the urethra.
How PEMF May Help:
- May contribute to modest prostate volume reduction (opening urethral channel)
- Potentially reduces tissue swelling
- Could improve muscle relaxation
- Potential Result: Stronger, more consistent flow
Difficulty Starting Urination (Hesitancy)
The Problem: Pressure on urethra plus bladder muscle dysfunction.
How PEMF May Help:
- May improve nerve-muscle communication
- Potentially reduces urethral resistance
- Could enhance bladder muscle function
- Potential Result: Easier initiation, less straining
Incomplete Bladder Emptying
The Problem: Enlarged prostate prevents complete voiding.
How PEMF May Help:
- May help shrink obstructing tissue modestly
- Potentially improves bladder contractility
- Could reduce post-void residual volume
- Potential Result: More complete emptying, fewer repeat trips
Nocturia (Nighttime Urination)
The Problem: Combination of incomplete emptying and bladder irritation.
How PEMF May Help:
- May reduce inflammation-related bladder irritation
- Potentially improves bladder capacity
- Could decrease urgency signals
- Potential Result: Fewer wake-ups, better sleep quality
Dribbling and Intermittent Stream
The Problem: Partial urethral obstruction and poor muscle coordination.
How PEMF May Help:
- May help open urethral passage
- Potentially improves sphincter control
- Could enhance flow consistency
- Potential Result: Cleaner, more complete stream
Note: These are proposed mechanisms based on the limited pilot study data. Individual results may vary significantly, and more research is needed to confirm these effects.
PEMF Treatment Protocols: What to Expect
Clinical PEMF Therapy
If you choose professional treatment, here's what a typical protocol might look like based on research parameters:
Treatment Parameters:
- Frequency: 2-3 sessions per week initially (though home protocols use daily treatment)
- Session duration: 20-30 minutes (pilot study used 5 minutes twice daily)
- Electromagnetic frequency: 1-50 Hz (typically 6-15 Hz for prostate applications)[11]
- Treatment course: 4-12 weeks based on pilot data
- Maintenance: To be determined - pilot study showed maintained effect at 4 months
What Happens During Treatment:
- You lie comfortably on a treatment table
- PEMF applicator is positioned over pelvic area
- You may feel gentle warmth or tingling (or nothing at all)
- You can read, relax, or even nap during treatment
- No discomfort or recovery time needed
Expected Timeline (Based on Pilot Study):
- Week 1-2: May notice reduced urgency in some patients
- Week 3-4: Improved flow, less nighttime urination reported
- Week 4-8: Potential for measurable prostate changes
- Week 8-12: Maximum symptom relief achieved in responders
Cost:
- Per session: $100-$300 (varies widely)
- Full treatment course: $1,200-$3,600
- Insurance typically does not cover investigational treatments
Home PEMF Therapy Devices
Many men prefer the convenience and privacy of home PEMF treatment based on the pilot study's self-administered approach. Here's what you need to know:
Device Types:
1. Full-Body PEMF Mats
- Pros: Treats multiple conditions, comfortable to use
- Cons: Less targeted to prostate
- Cost: $1,500-$4,000
- Best for: General wellness + prostate health
2. Targeted Pelvic PEMF Devices
- Pros: Focused treatment similar to research protocols
- Cons: Limited to pelvic area only
- Cost: $500-$2,000
- Best for: Dedicated prostate treatment (closest to study design)
3. Clinical-Grade Home Systems
- Pros: Most powerful, professional results at home
- Cons: Higher cost, larger equipment
- Cost: $4,000-$6,000
- Best for: Serious long-term investment
Key Features to Look For:
✅ Adjustable frequency settings (1-50 Hz range to match research parameters)
✅ Sufficient intensity (check device specifications)
✅ Pelvic-specific applicators or positioning
✅ FDA registration (for safety and quality)
✅ Programmable sessions with auto-shutoff
✅ Good warranty (at least 1-2 years)
✅ Customer support and training included
Home Treatment Protocol (Based on Research):
- Frequency: The pilot study used twice-daily sessions
- Duration: 5 minutes per session in the published study[11]
- Timing: Morning and evening for consistency
- Positioning: Perineal application (between scrotum and anus)
- Duration of treatment: Minimum 28 days based on research
Cost Analysis: PEMF vs. Traditional Treatments
5-Year Cost Comparison:
- PEMF Home Device: $2,500 (one-time) = $2,500 total
- Alpha-Blocker Medication: $100/month × 60 months = $6,000 total
- 5-ARI Medication: $75/month × 60 months = $4,500 total
- Combination Therapy: $150/month × 60 months = $9,000 total
- UroLift Procedure: $6,500 (may need repeat) = $6,500-$13,000 total
- Rezūm Therapy: $4,000 = $4,000 total
- TURP Surgery: $15,000 (one-time) = $15,000 total
PEMF may offer good long-term value if effective, especially considering:
- No ongoing prescription costs after device purchase
- Can potentially be used for other health conditions
- Family members may benefit from device
- No need for repeated doctor visits
However, remember that established treatments have much stronger evidence supporting their efficacy.
Who Should Consider PEMF Therapy for BPH?
Ideal Candidates for Exploration
PEMF therapy might be worth discussing with your doctor if you have:
Prostate Characteristics:
- Mild to moderate BPH (prostate size 30-80cc)
- Inflammation-suspected enlargement
- No acute urinary retention
- No significant bladder stones or damage
Health Status:
- Good overall health
- No pacemaker or implanted electronic devices (absolute contraindication)
- No active infections
- Realistic expectations about preliminary nature of evidence
Treatment Goals:
- Want to explore emerging non-invasive options
- Seeking complementary approaches
- Experiencing medication side effects
- Prefer to attempt conservative management first
- Willing to commit to daily treatment protocol
- Understanding this is investigational
When to Combine PEMF with Other Therapies
PEMF can potentially be safely combined with:
Lifestyle Modifications:
- Pelvic floor exercises (Kegels)
- Dietary changes (anti-inflammatory diet)
- Stress reduction
- Regular physical activity
- Weight management
Natural Supplements (Discuss with doctor):
- Saw palmetto
- Beta-sitosterol
- Pygeum africanum
- Pumpkin seed extract
Medications (Under physician guidance):
- May potentially be used alongside alpha-blockers for symptom relief
- Discuss any combination therapy with your urologist
- Monitor carefully for symptom changes
When Conventional Treatment Is Necessary
PEMF is not appropriate if you have:
- Severe BPH with complete urinary retention requiring catheterization
- Recurrent urinary tract infections due to incomplete bladder emptying
- Bladder stones or significant bladder damage
- Kidney damage (hydronephrosis) from obstruction
- Very large prostate (>100cc) with severe symptoms
- Hematuria (blood in urine) requiring investigation
- Elevated PSA requiring cancer workup
- Failed multiple conservative treatments without improvement
In these cases, discuss with your urologist whether PEMF could potentially be used after addressing acute issues or as an adjunct to prevent recurrence, but do not delay necessary medical or surgical treatment.
Enhancing Results: Complementary Strategies
To potentially maximize your outcomes with any BPH therapy, including PEMF, consider these evidence-based additions:
Pelvic Floor Exercises
Kegel Exercises for Men:
- Strengthen pelvic muscles
- May improve bladder control
- Can enhance urinary flow
- Simple to perform anywhere
How to Do Kegels:
- Identify muscles (stop urine mid-stream to feel them)
- Contract for 5 seconds, relax for 5 seconds
- Repeat 10-15 times, 3 times per day
- Practice when lying down, sitting, and standing
Dietary Modifications
Foods That May Support Prostate Health:
- Tomatoes - Rich in lycopene, an antioxidant
- Fatty fish - Omega-3 fatty acids with anti-inflammatory properties
- Green tea - Contains catechins that may reduce inflammation
- Cruciferous vegetables - Broccoli, cauliflower (sulforaphane)
- Berries - High in antioxidants
- Pumpkin seeds - Natural source of zinc
- Turmeric - Anti-inflammatory compound curcumin
Foods to Limit:
- Caffeine - Can irritate the bladder
- Alcohol - Increases urine production
- Spicy foods - May worsen urgency in some men
- High-sodium foods - Can cause fluid retention
- Red meat - Some studies suggest limiting consumption
Lifestyle Habits
Bladder-Friendly Practices:
- Don't hold urine too long (can weaken bladder muscles)
- Double-void technique (urinate twice, 30 seconds apart)
- Avoid drinking large amounts of fluids 2-3 hours before bed
- Take warm baths to relax pelvic muscles
- Manage stress (can increase urgency)
- Maintain healthy weight (obesity associated with worse BPH)[17]
- Stay physically active (regular exercise may help symptoms)
Targeted Supplements (Discuss with Your Doctor)
Evidence-Based Options:
Saw Palmetto (320mg daily)
- Some studies show benefit; others show no effect
- May reduce DHT levels in prostate
- Anti-inflammatory properties
- Consult doctor before use
Beta-Sitosterol (60-130mg daily)
- Plant sterol shown to improve urinary symptoms in some studies
- May reduce prostate inflammation
- Generally well-tolerated
Pygeum (100-200mg daily)
- African tree bark extract
- Some evidence for reducing nighttime urination
- Anti-inflammatory effects
Stinging Nettle (300-600mg daily)
- May help block DHT binding
- Reduces inflammation
- Often combined with saw palmetto
Note: Supplements are not regulated by FDA for efficacy. Discuss with your healthcare provider before starting any supplement regimen, especially if taking medications.
Safety and Contraindications
Is PEMF Therapy Safe?
PEMF has shown a good safety profile in published pilot studies:[11,12]
Safety Advantages:
- Non-thermal (doesn't heat tissue)
- No ionizing radiation
- No tissue destruction
- Reversible effects
- No drug interactions reported
- Can be stopped anytime without withdrawal
- High compliance rates in studies
Potential Mild Side Effects (Reported in Studies):
- Temporary increase in urination frequency (as prostate potentially shrinks)
- Mild pelvic warmth during treatment
- Occasional fatigue (body's healing response)
- These typically resolve within 1-2 weeks
No Serious Adverse Events were reported in the published pilot studies.[11,12]
Who Should Not Use PEMF
Absolute Contraindications:
- ⚠️ Pacemakers or implanted cardiac devices (electromagnetic interference)
- ⚠️ Insulin pumps or medication pumps (device malfunction risk)
- ⚠️ Cochlear implants (electromagnetic interference)
- ⚠️ Metal implants in treatment area (heating risk)
- ⚠️ Active bleeding or hemorrhage (may affect clotting)
Relative Contraindications (Consult Doctor First):
- Recent surgery (within 6 weeks) in treatment area
- Active infections or fever
- Pregnancy in household (if treating partner's device nearby)
- Epilepsy or seizure disorders (theoretical concern)
- Active cancer (insufficient data on PEMF effects)
- Bleeding disorders or anticoagulant therapy
Important Precautions
Before starting PEMF therapy:
- Get proper diagnosis - Ensure symptoms are from BPH, not prostate cancer or other conditions
- Baseline measurements - PSA test, digital rectal exam, urinalysis, flow study, post-void residual
- Medical consultation - Discuss with urologist; understand this is investigational
- Follow protocols - Use device according to research parameters and manufacturer guidelines
- Monitor progress - Track symptoms with validated questionnaires (IPSS)
- Regular follow-up - Continue medical monitoring even while using PEMF
- Report changes - Inform your doctor of any symptom worsening or new issues
Getting Started with PEMF Therapy for BPH
Step 1: Confirm Your Diagnosis
Essential Tests Before Any Treatment:
- Digital rectal exam (DRE) - Assess prostate size and texture
- PSA blood test - Rule out prostate cancer (normal <4 ng/mL typically)
- Urinalysis - Check for infection or blood
- Post-void residual measurement - How much urine remains after urinating
- Uroflowmetry - Measure urinary flow rate
- IPSS questionnaire - Standardize symptom assessment
Optional But Helpful:
- Transrectal ultrasound (TRUS) for accurate prostate volume
- Cystoscopy (if symptoms are severe or unclear diagnosis)
- Urodynamic testing (pressure-flow studies)
- Kidney function tests if retention suspected
Step 2: Discuss Options with Your Doctor
Important Conversation Points:
- Understand that PEMF is investigational with limited evidence
- Discuss whether you're a candidate based on symptom severity
- Review all established treatment options per AUA guidelines
- Consider PEMF as potential complementary or alternative approach
- Establish monitoring plan if you proceed
- Understand when conventional treatment becomes necessary
- Set realistic expectations based on pilot study data
Step 3: Choose Your Treatment Path
Option A: Clinical Treatment
- Find a provider offering PEMF for BPH (limited availability)
- Schedule initial consultation and evaluation
- Commit to treatment schedule (protocols vary)
- Plan for 8-12 weeks initial course
- Budget for professional treatment costs
Option B: Home Treatment
- Research reputable device manufacturers
- Look for devices similar to those used in research (perineal application, 1-50 Hz)
- Compare features, specifications, and costs
- Read user reviews and check company reputation
- Purchase from authorized dealer with good warranty
- Follow research-based protocols (5 min twice daily to start)
Option C: Wait for More Evidence
- Pursue established treatments with strong evidence
- Monitor PEMF research developments
- Consider PEMF later if larger trials show benefit
- This is a perfectly reasonable approach
Step 4: Set Realistic Expectations
What Current Research Suggests You Might Expect:
- Gradual improvement over 4-8 weeks in some patients
- Modest symptom reduction (varies by individual)
- Small prostate volume changes (5.4% median in pilot study)
- Best results may require consistent daily use
- Some men may not respond
- Effects maintained at 4 months in pilot study
What Not to Expect:
- Overnight miracle cure or dramatic results
- 100% elimination of all symptoms
- Guaranteed results (this is experimental)
- Results equivalent to surgery or established medications
- Replacement for emergency medical care
- Cure for severe BPH or complications
Step 5: Track Your Progress
Metrics to Monitor:
- IPSS score - Standardized symptom questionnaire (download online)
- Nighttime bathroom trips - Keep a voiding diary
- Urinary flow strength - Subjective scale 1-10 or timed voiding
- Daytime frequency - Number of voids per day
- Quality of life - Impact on daily activities
- PSA levels - Every 6-12 months per doctor
- Maximum flow rate - If possible, repeat uroflowmetry
Consider Follow-Up Testing at 8-12 Weeks:
- Repeat IPSS questionnaire
- Repeat uroflowmetry
- Post-void residual measurement
- Prostate ultrasound to measure volume change
- PSA and urinalysis
Step 6: Adjust and Optimize
If Results Are Slower Than Expected:
- Ensure proper device positioning (perineal application)
- Verify device settings match research parameters
- Check treatment consistency (twice daily)
- Add complementary therapies (exercise, diet, supplements)
- Discuss with doctor whether medication addition is appropriate
- Consider whether symptom expectations were realistic
If Results Are Encouraging:
- Continue daily protocol consistently
- Don't discontinue abruptly
- Monitor for sustained benefit
- Continue medical follow-up
- Consider maintenance protocol after initial course
If No Improvement After 12 Weeks:
- Discuss conventional treatment options with urologist
- Don't delay necessary medical care
- PEMF may not work for everyone
- Reevaluate diagnosis and severity
Real Results: What the Research Shows
While individual results will vary, here's what the published pilot study reported:[11]
Study Outcomes (28 Days of Treatment)
Prostate Volume:
- Median reduction: 5.4%
- Range of reduction: 3.2% to 12.8% among responders
- Maintained at 4-month follow-up
Symptom Improvement:
- Significant reduction in IPSS scores (lower urinary tract symptoms)
- Particularly in patients with moderate-severe symptoms
- Better outcomes in patients without metabolic syndrome
- High treatment compliance (>90%)
Safety and Tolerability:
- No serious adverse events
- No changes in testosterone levels
- No negative effects on sexual function (IIEF-15 scores)
- Well-tolerated by all participants
Important Study Limitations
What This Study Does NOT Tell Us:
- Long-term efficacy beyond 4 months
- Results in very large prostates (>80cc)
- Comparison to placebo or sham treatment
- Optimal treatment duration or frequency
- Results in diverse populations (study was Italian Caucasians)
- Cost-effectiveness compared to standard treatments
- Whether improvements continue beyond 4 months
Study Weaknesses:
- Very small sample size (27 patients)
- No control group (all patients received treatment)
- No blinding (patients knew they were being treated)
- Funded by device manufacturer (Parsemus Foundation)
- Single-center study
- Short follow-up period
What Doctors Are Saying
The medical community recognizes PEMF as promising but preliminary:
- "The pilot study provided promising evidence for the usefulness of PEMF to treat BPH. Additional research with a larger number of men and a control group is needed."[14]
- Current AUA guidelines do not include PEMF as a recommended treatment due to insufficient evidence[9]
- More research is needed to understand optimal treatment schedules and long-term outcomes[11]
The Future of Non-Surgical BPH Treatment
PEMF therapy represents a potential shift in how we might approach enlarged prostate treatment. Rather than simply managing symptoms with drugs or destroying tissue with surgery, electromagnetic therapy offers a potentially restorative approach that:
- May address root inflammatory causes
- Preserves natural tissue and function
- Avoids systemic side effects
- Can potentially be self-administered at home
- Shows promise in early research
However, it's crucial to maintain realistic expectations. PEMF is not yet proven as an established treatment for BPH. Larger, well-designed clinical trials with control groups are essential before this therapy can be recommended as standard care.
What's Needed Moving Forward
Research Priorities:
- Large randomized controlled trials with placebo/sham groups
- Longer-term follow-up (1-2 years minimum)
- Head-to-head comparisons with established treatments
- Optimal treatment parameters and protocols
- Identification of which patients respond best
- Cost-effectiveness analyses
- Quality of life assessments with validated instruments
Current Status
- Evidence level: Preliminary (small pilot studies only)
- AUA guideline status: Not included
- Insurance coverage: Generally not covered
- Availability: Limited; mainly through research or specialty clinics
- FDA status: PEMF devices may be FDA-registered for general wellness, not specifically approved for BPH treatment
Key Takeaways
✅ PEMF is an emerging, investigational approach for enlarged prostate
✅ Pilot studies show encouraging results but are preliminary
✅ 5.4% median prostate shrinkage in 28 days in one small study
✅ Symptom improvement reported in patients without metabolic syndrome
✅ Treatment appears safe with minimal side effects in published studies
✅ Non-invasive approach with no impact on sexual function
✅ Much more research needed before becoming standard of care
✅ Not a replacement for established treatments in moderate-severe BPH
✅ Best used with medical supervision and realistic expectations
Take Action: Making an Informed Decision
If you're struggling with an enlarged prostate, you have several evidence-based options. PEMF therapy is an emerging technology that shows promise but remains investigational.
We recommend:
- Discuss all options with your urologist - Review the full spectrum from watchful waiting to medications to procedures
- Understand the evidence levels - Established treatments have decades of research; PEMF has small pilot studies
- Consider your symptom severity - Mild symptoms may allow time to explore newer options; severe symptoms need proven treatments
- Set realistic expectations - PEMF may help some patients but is not a proven cure
- Don't delay necessary care - If you have complications (retention, kidney damage), pursue established treatments
- Stay informed - Monitor medical literature for new PEMF studies as they emerge
Ready to learn more? Watch the video above to see PEMF therapy in action, and consult with a qualified healthcare provider to develop your personalized treatment plan that's right for your specific situation.
The path to better prostate health doesn't have to involve scalpels or lifelong medications for everyone. With PEMF therapy and other emerging approaches, combined with established treatments, you may have more options than ever before. However, always work closely with your medical team to make the best decision based on your individual circumstances and the current state of scientific evidence.
References and Scientific Sources
Primary PEMF Therapy Studies
- Tenuta M, Tarsitano MG, Mazzotta P, Lucchini L, Sesti F, Fattorini G, Pozza C, Olivieri V, Naro F, Gianfrilli D, Lenzi A, Isidori AM, Pofi R. Therapeutic use of pulsed electromagnetic field therapy reduces prostate volume and lower urinary tract symptoms in benign prostatic hyperplasia. Andrology. 2020 Aug;8(4):997-1005. doi:10.1111/andr.12775
https://pubmed.ncbi.nlm.nih.gov/32090492/
https://pmc.ncbi.nlm.nih.gov/articles/PMC7496682/ - Leoci R, Aiudi G, Silvestre F, Lissner EA, Marino F, Lacalandra GM. Effect of Pulsed Electromagnetic Field Therapy on Prostate Volume and Vascularity in the Treatment of Benign Prostatic Hyperplasia: A Pilot Study in a Canine Model. The Prostate. 2014 Aug;74(11):1132-1141. doi:10.1002/pros.22824
https://pmc.ncbi.nlm.nih.gov/articles/PMC4145661/ - Parsemus Foundation. PEMF Therapy for Enlarged Prostate. Updated September 2025.
https://www.parsemus.org/humanhealth/treatment-for-enlarged-prostate/
BPH Pathophysiology and Inflammation Research
- Inamura S, Kato M, Sugiura M, Goya N, Fukuhara H. Chronic inflammation in benign prostatic hyperplasia: Pathophysiology and treatment options. International Journal of Urology. 2024 Aug;31(8):816-827. doi:10.1111/iju.15518
https://pmc.ncbi.nlm.nih.gov/articles/PMC11524144/ - Fibbi B, Penna G, Morelli A, Adorini L, Maggi M. Chronic inflammation in the pathogenesis of benign prostatic hyperplasia. International Journal of Andrology. 2010 Jun;33(3):475-488. doi:10.1111/j.1365-2605.2009.00972.x
https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2605.2009.00972.x - Ghafar MA, Anastasiadis AG, Chen MW, et al. Acute hypoxia increases the aggressive characteristics and survival properties of prostate cancer cells. Prostate. 2003;54(1):58-67.
- Kramer G, Mitteregger D, Marberger M. Is benign prostatic hyperplasia (BPH) an immune inflammatory disease? European Urology. 2007;51(5):1202-1216.
- Nickel JC. Inflammation and Benign Prostatic Hyperplasia. Urologic Clinics of North America. 2008 Feb;35(1):109-115. doi:10.1016/j.ucl.2007.09.012
https://pmc.ncbi.nlm.nih.gov/articles/PMC2198849/ - Foster HE, Barry MJ, Dahm P, Gandhi MC, Kaplan SA, Kohler TS, Lerner LB, Lightner DJ, Parsons JK, Roehrborn CG, Welliver C, Wilt TJ, McVary KT. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia (BPH): AUA Guideline Amendment 2023. Journal of Urology. 2023 Nov;210(5):767-776. doi:10.1097/JU.0000000000003698
https://www.auanet.org/guidelines-and-quality/guidelines/benign-prostatic-hyperplasia-(bph)-guideline - Parsons JK, Dahm P, Köhler TS, Lerner LB, Wilt TJ. Surgical Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA Guideline Amendment 2020. Journal of Urology. 2020 Oct;204(4):799-804.
https://www.auanet.org/documents/guidelines/pdf/bph-surgical-management-2020.pdf - Tenuta M, et al. [Full citation repeated from #1 above for easy reference to main study]
- Leoci R, et al. [Full citation repeated from #2 above for easy reference to canine study]
- De Nunzio C, Kramer G, Marberger M, et al. The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. European Urology. 2011;60(1):106-117.
- Parsemus Foundation. Electromagnetic therapy effective for enlarged prostate. Press Release. April 2020.
https://www.parsemus.org/2020/04/electromagnetic-therapy-effective-for-enlarged-prostate/ - Giannakopoulos X, Baltogiannis D, Giannakis D, et al. Short-term efficacy of the magnetic field in the treatment of benign prostatic hyperplasia. International Urology and Nephrology. 2011;43(4):1097-1103.
- Elgohary H, Tantawy SA. Efficacy of pulsed high-intensity laser therapy on pain, functional capacity, and quality of life in patients with chronic prostatitis: a randomized placebo-controlled study. Lasers in Medical Science. 2017;32(3):583-589.
Additional BPH Research
- Devlin CM, Simms MS, Maitland NJ. Benign prostatic hyperplasia – what do we know? BJU International. 2021 Feb;127(4):389-399. doi:10.1111/bju.15229
https://bjui-journals.onlinelibrary.wiley.com/doi/10.1111/bju.15229 - Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. Journal of Urology. 1984;132(3):474-479.
- Roehrborn CG. Benign prostatic hyperplasia: an overview. Reviews in Urology. 2005;7(Suppl 9):S3-S14.
General Medical References
- StatPearls [Internet]. Benign Prostatic Hyperplasia. Updated October 2024. Treasure Island (FL): StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK558920/ - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Prostate Enlargement (Benign Prostatic Hyperplasia). Updated 2021.
https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia - Mayo Clinic. Benign Prostatic Hyperplasia (BPH): Symptoms and Causes. Updated 2024.
https://www.mayoclinic.org/diseases-conditions/benign-prostatic-hyperplasia/ - Barry MJ, Fowler FJ Jr, O'Leary MP, et al. The American Urological Association Symptom Index for Benign Prostatic Hyperplasia. Journal of Urology. 2017 Feb;197(2S):S189-S197.
Additional Resources for Patients
American Urological Association - Urology Care Foundation
Patient Guide to BPH: https://www.urologyhealth.org/urology-a-z/b/benign-prostatic-hyperplasia-(bph)
National Kidney and Urologic Diseases Information Clearinghouse
https://www.niddk.nih.gov/health-information/urologic-diseases
Prostate Conditions Education Council
https://www.prostateconditions.org/
International Prostate Symptom Score (IPSS) Calculator
Available through urologyhealth.org and various medical websites
Disclaimer: This article is for educational purposes only and does not constitute medical advice. The PEMF therapy studies cited represent preliminary research with small sample sizes and significant limitations. PEMF is not currently included in standard medical guidelines for BPH treatment and should be considered investigational. Large-scale randomized controlled trials are needed to establish efficacy, safety, optimal protocols, and appropriate patient selection. Always consult with a qualified healthcare provider before beginning any new treatment for benign prostatic hyperplasia (BPH). Do not delay necessary medical or surgical care while exploring investigational treatments.