Electromagnetic Therapy for Pelvic Floor Dysfunction: What Recent Clinical Studies Reveal
If you've been following developments in pelvic electromagnetic field (PEMF) therapy, you've probably noticed something: while there's plenty of general wellness marketing around electromagnetic therapy, specific medical applications backed by peer-reviewed research are harder to find.
That's changing—particularly in the area of women's pelvic floor health.
Two recent clinical studies have evaluated electromagnetic therapy for specific pelvic floor conditions: stress urinary incontinence (SUI) and pelvic organ prolapse (POP). Unlike promotional materials or testimonials, these are actual peer-reviewed studies from medical centers, with measured outcomes and published results.
Let's break down what the research actually shows.
The Scope of the Problem: Why Pelvic Floor Disorders Matter
Before diving into the studies, it's worth understanding just how common—and impactful—pelvic floor disorders are.
The statistics are striking:
- Approximately 50% of women who have given birth will experience some degree of pelvic floor dysfunction in their lifetime
- Stress urinary incontinence affects up to 35% of women over age 30
- Pelvic organ prolapse occurs in 30-50% of women who have had children
- These conditions have a quality of life impact comparable to chronic diseases like arthritis, diabetes, and heart disease
Yet despite how common these issues are, many women suffer in silence due to embarrassment or believing "this is just part of getting older."
Current treatment options include:
- Pelvic floor muscle training (PFMT) - Effective but requires significant patient effort, proper technique, and ongoing compliance
- Vaginal pessaries - Mechanical support devices that work for some women but can be uncomfortable
- Surgery - Highly effective but invasive, with risks and recovery time
There's clearly a need for non-invasive options that don't require the intensive commitment of PFMT or the risks of surgery.
That's where electromagnetic therapy enters the picture.
How Electromagnetic Pelvic Floor Therapy Works
Before looking at the research, let's understand the mechanism.
Flat magnetic stimulation (FMS) devices use time-varying electromagnetic fields to induce muscle contractions in the pelvic floor. Unlike traditional electrical stimulation (which requires vaginal or rectal probes), electromagnetic therapy works through clothing.
The proposed mechanism:
- The device generates pulsed electromagnetic fields
- These fields penetrate deep into pelvic tissue (several centimeters)
- The changing magnetic field induces electrical currents in conductive tissue
- This causes depolarization of nerve and muscle cells
- Result: Involuntary contraction of pelvic floor muscles
Theoretical advantages:
- Non-invasive - No internal probes required
- Passive treatment - Patient sits fully clothed; no active effort needed
- Deep penetration - Can reach muscles difficult to activate voluntarily
- Comfortable - Generally well-tolerated with minimal side effects
- Compliance-friendly - Easier to stick with than exercises requiring daily discipline
Now let's see what happens when this theory is put to the test in actual clinical studies.
📧 For Healthcare Practitioners
Are you a urogynecologist, pelvic floor physical therapist, or women's health specialist interested in learning more about electromagnetic therapy for your practice?
We provide evidence-based information and clinical support for practitioners considering electromagnetic pelvic floor rehabilitation options, including the QRS-1010 PelviCenter.
Contact us for:Complete clinical evidence packageTreatment protocol guidelinesPractice implementation supportDevice demonstrationsContinuing education resources
Email: [email protected]
Subject Line: "Practitioner Inquiry - Pelvic Floor EM Therapy"
We respond to all practitioner inquiries within 24 hours.
Study #1: Pelvic Organ Prolapse (2025)
The most recent published research comes from Italy and was published in December 2025.
Study Details:
Citation: De Vicari D, Barba M, Cola A, Amatucci N, Carrara S, Frigerio M. Flat Magnetic Stimulation in the Conservative Management of Mild Pelvic Organ Prolapse: A Retrospective Observational Study. Medicina. 2025;61(12):2198.
Institution: Department of Gynecology, IRCCS San Gerardo dei Tintori, University of Milano-Bicocca, Italy
Study Design: Retrospective observational study
Participants: 87 women with stage ≤2 pelvic organ prolapse (mild POP)
Treatment Protocol:
- 8 sessions of electromagnetic stimulation
- 25 minutes per session
- Twice weekly for 4 consecutive weeks
- Device: Dr. Arnold chair (DEKA, Calenzano, Italy)
Outcome Measures:
- Primary: Anatomical changes measured using the POP-Q (Pelvic Organ Prolapse Quantification) system - the international gold standard for measuring prolapse
- Secondary: Patient-reported improvement using the PGI-I (Patient Global Impression of Improvement) questionnaire
The Results:
Anatomical Outcomes:
The study found statistically significant improvements in the anterior vaginal compartment:
- Aa point: Improved from -0.3±1.2 cm to -0.7±1.3 cm (p=0.03)
- Ba point: Improved from -0.3±1.3 cm to -0.7±1.3 cm (p=0.04)
These measurements indicate elevation of the anterior vaginal wall—meaning the prolapse improved measurably.
For those not familiar with POP-Q measurements, these are standardized reference points measured in centimeters relative to the vaginal opening. Negative numbers indicate the tissue is above the opening (better support), while positive numbers indicate descent below the opening (prolapse).
Patient-Reported Outcomes:
Perhaps more importantly for quality of life, the subjective results were strong:
- 90.8% of patients (79 out of 87) reported some degree of symptomatic improvement
- 37.9% rated themselves as "very much improved" or "much improved"
- 52.9% reported being "minimally improved"
- Only 9.2% reported no change
- Zero patients reported worsening of their condition
Safety Profile:
- 100% treatment compliance - All 87 women completed all 8 sessions
- Zero adverse events reported
- No discomfort or complications noted during or after treatment
What This Means:
This study demonstrates that electromagnetic stimulation can produce both objective anatomical improvements (measured with standardized tools) and subjective symptom relief (patient-reported outcomes) in women with mild pelvic organ prolapse.
The fact that 100% of participants completed treatment and no one experienced adverse effects suggests this is a well-tolerated intervention.
Important limitations the researchers acknowledge:
- Retrospective design - No control group, so we can't rule out placebo effects
- Short follow-up - Only 1 week after treatment completion; longer-term durability unknown
- Modest anatomical changes - While statistically significant, the clinical significance of 0.4cm improvement is debatable
- Anterior compartment only - No significant improvements seen in apical or posterior prolapse
The researchers appropriately conclude that while results are promising, prospective randomized controlled trials with longer follow-up are needed.
Study #2: Stress Urinary Incontinence (2015)
The second study addresses a different but related condition: stress urinary incontinence.
Study Details:
Citation: Lim R, Liong ML, Leong WS, Khan NAK, Yuen KH. Magnetic stimulation for stress urinary incontinence: study protocol for a randomized controlled trial. Trials. 2015;16:279.
Institution: Universiti Sains Malaysia, in collaboration with multiple hospitals in Northern Malaysia
Study Design: Multicenter, randomized, double-blind, sham-controlled, parallel-group trial
Sample Size: 120 women with stress urinary incontinence (planned enrollment)
Treatment Protocol:
- 16 sessions total (2 sessions per week for 8 weeks)
- 20 minutes per session
- Device: QRS-1010 PelviCenter (QRS International, Liechtenstein)
Critical Design Element - Sham Control:
This study includes a particularly rigorous placebo control. The sham group receives:
- Same device, same appearance and sound
- Magnetic coil tilted to 22° down
- Lower intensity stimulation (max 60% vs. 100%)
- Total energy output far less than active treatment
This addresses a major weakness in many electromagnetic therapy studies: proper blinding and placebo control.
Outcome Measures:
Primary:
- ICIQ-UI-SF (International Consultation on Incontinence Questionnaire for Urinary Incontinence Short Form) - a validated, Grade A outcome measure
- Response defined as 5+ point reduction from baseline
Secondary:
- Cure rate (objective: <1g leakage on pad test; subjective: "never" leaking)
- Incontinence episode frequency (50%+ reduction)
- 1-hour pad test (50%+ reduction in pad weight)
- Pelvic floor muscle strength (perineometer measurement)
- Quality of life measures (PGI-I, ICIQ-LUTS-QoL, EQ-5D)
The Study's Significance:
While this publication is the study protocol (not results), it's worth noting for several reasons:
- Rigorous methodology - Double-blind, sham-controlled design is the gold standard
- Validated outcomes - Uses internationally recognized, psychometrically tested measures
- Adequate sample size - Powered to detect clinically meaningful differences
- Cost-effectiveness analysis - Plans to evaluate not just efficacy but economic value
The study was registered on ClinicalTrials.gov (NCT01924728), demonstrating transparency and pre-registration of methodology—a mark of high-quality research.
Important Note:
This 2015 paper describes the study design and methodology. As of this writing, I could not locate published results from this trial in peer-reviewed literature. This could mean:
- Results are pending publication
- The study was completed but results were negative or inconclusive (less likely to be published)
- The study encountered enrollment or completion challenges
The methodology itself is exemplary and shows what high-quality research in this area should look like. If you're considering electromagnetic therapy for SUI, it would be worth checking whether results from this trial have since been published.
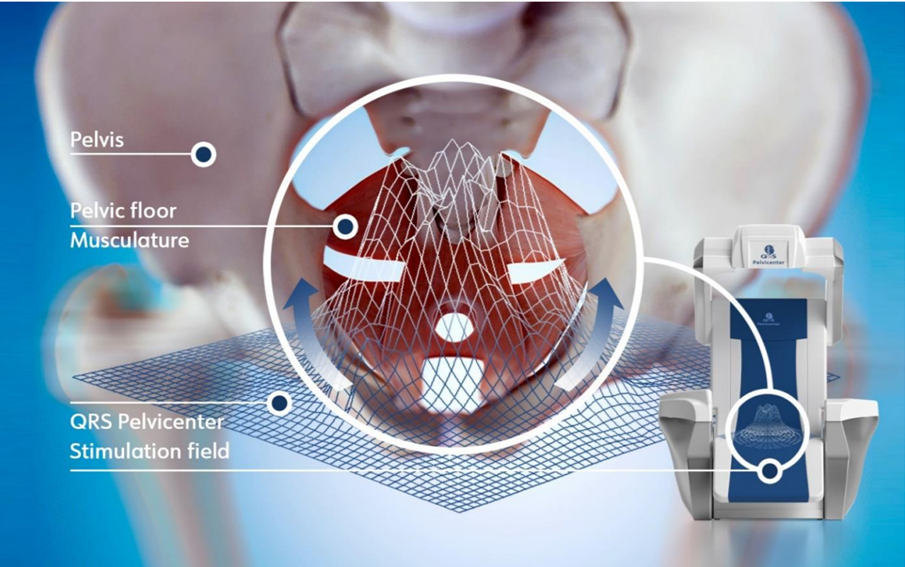
The QRS-1010 PelviCenter: Device Used in the SUI Study
The Malaysian randomized controlled trial used the QRS-1010 PelviCenter (QRS International, Liechtenstein), a medical electromagnetic chair specifically designed for pelvic floor rehabilitation.
Key Features of the QRS-1010 PelviCenter:
- Seated treatment - Patients remain fully clothed
- Electromagnetic field technology - Penetrates deep into pelvic floor tissues
- Programmable protocols - Adjustable intensity and frequency settings
- Non-invasive - No internal probes or physical contact required
- Clinical heritage - Technology reportedly in use since 1998 in various markets
Treatment Experience:
During a typical PelviCenter session:
- Patient sits comfortably in the chair
- Electromagnetic field generates involuntary pelvic floor muscle contractions
- Sensation is typically described as tingling or pulsing in the pelvic area
- Sessions last 20-25 minutes
- No recovery time needed - patients can resume normal activities immediately
Who Might Benefit:
Based on the study protocol, potential candidates include women with stress urinary incontinence who:
- Have difficulty performing PFMT correctly
- Struggle with long-term PFMT compliance
- Prefer passive treatment options
- Are not candidates for surgery
- Want to avoid internal devices
Important Caveat:
While the Lim study protocol is published and demonstrates rigorous methodology, the results of this specific trial have not yet appeared in peer-reviewed literature. This means we know the PelviCenter was used in a well-designed study, but we don't yet have published outcomes data from that trial.
For practitioners interested in electromagnetic therapy using the PelviCenter technology, it's worth noting that the device shares similar mechanism of action principles with the device used in the De Vicari pelvic organ prolapse study, though they are manufactured by different companies.
What Makes These Studies Different From Marketing Claims
If you've spent any time researching PEMF therapy, you've probably encountered a lot of marketing materials that claim "research-backed" or "clinically proven" benefits.
So what makes these studies different?
1. Peer-Reviewed Publication
Both studies were published in peer-reviewed medical journals:
- Medicina - An MDPI journal indexed in major databases
- Trials - A well-respected open-access journal dedicated to randomized trials
This means independent scientists reviewed the methodology, analyzed the data, and deemed it worthy of publication.
2. Credible Institutions
These weren't industry-funded marketing studies:
- University of Milano-Bicocca (Italy) - A recognized academic medical center
- Universiti Sains Malaysia - A major research university
3. Specific, Measurable Outcomes
Instead of vague claims, these studies used:
- POP-Q measurements - The international gold standard for quantifying prolapse, measured in centimeters with statistical analysis
- Validated questionnaires - Tools that have undergone extensive psychometric testing (ICIQ-UI-SF, PGI-I)
- Objective measures - Pad tests, perineometer readings
4. Transparent About Limitations
The De Vicari study explicitly states:
- The retrospective design is a limitation
- Short follow-up period
- Clinical significance of small anatomical changes is uncertain
- More research needed
This honest acknowledgment of limitations is the hallmark of good science.
5. No "Miracle Cure" Claims
The researchers position electromagnetic therapy as:
- "A safe, well-tolerated, and potentially effective conservative therapy"
- An adjunct or alternative to PFMT, not a replacement for all treatment
- Appropriate for specific patient populations (mild POP, SUI)
This measured language contrasts sharply with marketing materials claiming electromagnetic therapy "treats" dozens of unrelated conditions.
What These Studies DON'T Show
In the interest of balanced reporting, it's important to acknowledge what we still don't know:
1. Long-Term Durability
The De Vicari study followed patients for only 1 week after treatment ended. Critical questions remain:
- Do the improvements persist at 3 months? 6 months? 1 year?
- Is maintenance therapy required?
- Do benefits plateau or continue to improve?
2. Comparison to Standard Care
Neither study directly compared electromagnetic therapy to:
- Pelvic floor muscle training (PFMT) - the current first-line treatment
- Surgery
- Combined approaches (PFMT + electromagnetic therapy)
We don't know if electromagnetic therapy is:
- Better than PFMT
- Equivalent to PFMT
- An effective add-on to PFMT
3. Mechanism of Action
While the proposed mechanism (electromagnetic field → muscle contraction → strengthening) is plausible, these studies don't prove how the therapy works.
It's possible that benefits come from:
- Increased pelvic floor muscle strength
- Improved neuromuscular coordination
- Placebo effect (especially for subjective measures)
- Some combination
4. Optimal Treatment Parameters
Questions remain about:
- Ideal session duration and frequency
- Total number of sessions needed
- Intensity/strength of electromagnetic field
- Which patients are most likely to benefit
5. Cost-Effectiveness
While the Lim protocol planned cost-effectiveness analysis, comparative economic data is lacking.
6. Broader Applicability
Both studies focused on:
- Women - No male pelvic floor dysfunction data
- Mild conditions - Stage ≤2 prolapse, pure stress incontinence
- No severe comorbidities - Exclusion criteria ruled out many real-world patients
We can't extrapolate these results to more severe cases or mixed urinary incontinence.
The Bigger Picture: Where Does Electromagnetic Therapy Fit?
Given the evidence, where does electromagnetic therapy belong in the treatment landscape for pelvic floor disorders?
A Reasonable Position:
Electromagnetic therapy appears to be a safe, non-invasive option that may benefit some women with mild pelvic floor dysfunction, particularly those who:
- Are not candidates for surgery
- Find PFMT challenging due to inability to identify/contract pelvic floor muscles properly
- Have trouble maintaining compliance with PFMT protocols
- Prefer passive treatments
- Want to avoid invasive procedures (pessaries, internal probes)
It's probably NOT:
- A replacement for PFMT in motivated patients
- Appropriate as first-line therapy for severe prolapse or incontinence
- An alternative to surgery when surgery is clearly indicated
- A treatment for the multiple unrelated conditions some marketing claims suggest
The Best Approach May Be Combination Therapy
Several pelvic floor experts have suggested that electromagnetic therapy might work best in combination with PFMT rather than as a standalone treatment.
The rationale:
- Electromagnetic therapy provides passive muscle stimulation and may help women learn to identify their pelvic floor
- PFMT teaches voluntary control and functional patterns
- Together, they may be more effective than either alone
This hasn't been rigorously tested yet, but it's a promising area for future research.
Clinical Implementation Considerations
For practitioners evaluating electromagnetic therapy options for their practice, devices like the QRS-1010 PelviCenter represent a clinical-grade approach that has been incorporated into the research protocols of peer-reviewed studies.
Key considerations for practice integration:
Patient Selection:
- Mild to moderate stress urinary incontinence
- Stage 1-2 pelvic organ prolapse
- Patients who have not responded adequately to PFMT alone
- Those seeking non-invasive alternatives to surgery
- Patients with PFMT compliance challenges
Treatment Protocols: Based on published research, typical protocols include:
- Frequency: 2 sessions per week
- Duration: 8 weeks (16 total sessions)
- Session length: 20-25 minutes
- Follow-up: Reassessment at 4 weeks, 8 weeks, and 3-6 months
Outcome Measurement: Essential to track objective measures:
- POP-Q measurements (for prolapse)
- Pad test results (for incontinence)
- Validated questionnaires (ICIQ-UI-SF, PGI-I)
- Perineometer readings (muscle strength)
Practice Economics:
- Device investment vs. per-treatment revenue
- Insurance coverage considerations (varies by payer and region)
- Patient out-of-pocket costs
- Competitive differentiation in your market
For detailed practice implementation guidance, contact [email protected]
Questions to Ask if Considering Electromagnetic Therapy
If you or someone you know is considering electromagnetic therapy for pelvic floor dysfunction, here are informed questions to ask providers:
About the Device:
- What specific device is being used?
- Does it have regulatory clearance (FDA/CE marking) for pelvic floor indications?
- What published research exists specifically for this device?
About the Treatment:
- What is the proposed treatment protocol (sessions, frequency, duration)?
- Is this based on published research or clinical experience?
- What outcomes can I reasonably expect?
- How will progress be measured?
About Alternatives:
- Have I tried PFMT with a trained pelvic floor physical therapist?
- How does electromagnetic therapy compare to standard treatments?
- Could I combine electromagnetic therapy with PFMT?
About Costs:
- What is the total cost?
- Is this covered by insurance?
- What is the cost compared to PFMT or other options?
About the Provider:
- What training do you have in pelvic floor disorders?
- How many patients have you treated with this therapy?
- Can you share outcome data from your patient population?
Equipment Considerations: What Practitioners Should Know
If you're a healthcare provider considering adding electromagnetic therapy to your pelvic floor treatment options, understanding the equipment landscape is important.
Different Devices, Similar Technology
The two studies discussed in this article used different manufacturers' devices:
- De Vicari study (2025): Dr. Arnold chair (DEKA, Italy)
- Lim study (2015 protocol): QRS-1010 PelviCenter (QRS International, Liechtenstein)
Both use flat magnetic stimulation technology with similar underlying principles, though specific engineering, field strength, and programmability may vary.
The QRS-1010 PelviCenter in Clinical Practice
For practitioners specifically interested in the QRS-1010 PelviCenter:
What We Know:
- ✅ Used in registered randomized controlled trial (NCT01924728)
- ✅ Rigorous study methodology published in peer-reviewed journal
- ✅ Protocol designed with validated outcome measures
- ✅ Technology has been commercially available in various markets
- ✅ Non-invasive, patient-friendly design
What We're Waiting For:
- ⏳ Published results from the Lim RCT
- ⏳ Long-term follow-up data
- ⏳ Head-to-head comparison studies
- ⏳ Larger-scale clinical trials
Regulatory Status:
It's essential for practitioners to verify current regulatory status for any medical device:
- Confirm FDA clearance status (if marketing in the US)
- Verify specific cleared indications
- Check CE marking documentation (for European markets)
- Understand any limitations or contraindications
Due Diligence for Practitioners:
Before adding any electromagnetic therapy device to your practice, we recommend:
- Request complete documentation:
- Regulatory clearances and 510(k) numbers
- Published clinical studies specific to the device
- Treatment protocols and guidelines
- Training and support programs
- Evaluate the evidence:
- Is the research peer-reviewed?
- Are results published or just protocols?
- Do studies use validated outcome measures?
- Are limitations honestly disclosed?
- Consider practice fit:
- Patient population needs
- Complementary to existing services
- Space and logistical requirements
- Staff training needs
- Financial analysis:
- Total cost of ownership
- Revenue per treatment
- Break-even analysis
- Insurance reimbursement landscape
Get Expert Guidance:
Making an informed decision about practice equipment investment requires comprehensive information. We provide consultative support to help practitioners evaluate options objectively.
Contact us for:
- Independent device comparisons
- Evidence review and interpretation
- Practice integration planning
- Regulatory documentation review
- ROI modeling specific to your practice
Email: [email protected]
Subject: "Practice Equipment Consultation"
What's Next for Electromagnetic Pelvic Floor Therapy?
Based on the current evidence, here's what we need:
Research Priorities:
- Large-scale RCTs - Like the Lim protocol, but with published results
- Head-to-head comparisons - Electromagnetic therapy vs. PFMT vs. combined approach
- Long-term follow-up - Minimum 12 months, ideally 2-3 years
- Optimal protocols - Dose-finding studies to determine ideal treatment parameters
- Predictive factors - Which patients are most likely to benefit?
- Mechanism studies - Neurophysiological measurements, MRI changes, EMG analysis
- Cost-effectiveness - Comparative economic analyses
Clinical Implementation:
For electromagnetic therapy to move from "promising experimental treatment" to "standard care option," we need:
- Clear clinical practice guidelines
- Insurance coverage decisions based on evidence
- Training standards for providers
- Patient selection criteria
- Integration with existing pelvic floor rehabilitation programs
The Bottom Line
The recent research on electromagnetic therapy for pelvic floor dysfunction shows promising but preliminary results.
What we know:
- ✅ Appears safe (zero adverse events in published study)
- ✅ Well-tolerated (100% compliance)
- ✅ May provide measurable anatomical improvements (in mild prolapse)
- ✅ High patient satisfaction (90.8% reported improvement)
- ✅ Non-invasive and convenient
- ✅ Rigorous study protocols have been designed and implemented
What we don't know:
- ❓ Long-term effectiveness
- ❓ How it compares to PFMT
- ❓ Optimal treatment protocols
- ❓ Which patients benefit most
- ❓ Cost-effectiveness
- ❓ Results from some key clinical trials (still pending publication)
The verdict:
For women with mild pelvic organ prolapse or stress urinary incontinence who are seeking non-invasive treatment options, electromagnetic therapy represents a reasonable consideration—especially for those who have struggled with PFMT or prefer passive treatments.
However, it should be:
- Provided by qualified practitioners
- Part of a comprehensive pelvic floor assessment
- Considered alongside (not instead of) other evidence-based treatments
- Measured with objective outcomes
- Re-evaluated if not showing benefit after reasonable trial
Most importantly, any provider offering electromagnetic therapy should be honest about what the evidence does and doesn't show, transparent about costs, and willing to discuss how this fits into your overall treatment plan.
For Patients: Finding Qualified Providers
If you're interested in electromagnetic therapy for pelvic floor concerns:
- Start with proper diagnosis - See a urogynecologist or pelvic floor physical therapist first
- Ask about all options - Including PFMT, pessaries, and electromagnetic therapy
- Request evidence - Ask providers what research supports their recommendations
- Verify qualifications - Ensure the provider has specific pelvic floor training
- Understand costs - Get clear pricing and insurance coverage information
For Healthcare Practitioners: Clinical Support
If you're a provider interested in incorporating evidence-based electromagnetic pelvic floor therapy into your practice, we offer comprehensive clinical and business support.
We assist with:
- ✓ Clinical evidence review and interpretation
- ✓ Device selection and vendor evaluation
- ✓ Treatment protocol development
- ✓ Staff training programs
- ✓ Patient selection criteria
- ✓ Outcome measurement tools
- ✓ Practice marketing support
- ✓ Insurance and reimbursement guidance
Our focus: Helping practitioners make informed, evidence-based decisions about pelvic floor rehabilitation technology, including the QRS-1010 PelviCenter and other electromagnetic therapy options.
📧 Contact: [email protected]
For Practitioners: Email with "Practitioner Consultation" in subject line
For Patients: Email with "Patient Information" in subject line
We respond to all inquiries within 24 hours and maintain strict confidentiality.
A Note on Evidence-Based Practice
This article represents our commitment to honest, evidence-based reporting on PEMF and electromagnetic therapy applications.
Our approach:
- We only cite peer-reviewed research
- We acknowledge limitations and unknowns
- We distinguish between marketing claims and clinical evidence
- We update content as new research emerges
Why this matters:
The PEMF and electromagnetic therapy field has a credibility problem. Too many providers make broad, unsubstantiated claims. Too many devices are marketed based on testimonials rather than rigorous research.
By focusing on specific, well-studied applications like pelvic floor dysfunction—where we have actual peer-reviewed studies with measured outcomes—we aim to elevate the conversation and help both practitioners and patients make informed decisions.
Stay informed:
This is an evolving field. New studies are being published regularly. We'll continue to monitor the research and update our readers on:
- New clinical trial results
- Comparative effectiveness studies
- Long-term outcome data
- Practice guidelines and protocols
Subscribe to our newsletter to receive updates when new research is published.
References
- De Vicari D, Barba M, Cola A, Amatucci N, Carrara S, Frigerio M. Flat Magnetic Stimulation in the Conservative Management of Mild Pelvic Organ Prolapse: A Retrospective Observational Study. Medicina. 2025;61(12):2198. doi:10.3390/medicina61122198 Open Access - Read Full Study
- Lim R, Liong ML, Leong WS, Khan NAK, Yuen KH. Magnetic stimulation for stress urinary incontinence: study protocol for a randomized controlled trial. Trials. 2015;16:279. doi:10.1186/s13063-015-0803-1 Open Access - Read Full Study
- Hagen S, Stark D, Glazener C, et al. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet. 2014;383(9919):796-806.
- Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654.
Want to Learn More?
Have questions about pelvic floor health or electromagnetic therapy? Drop them in the comments below. I read and respond to every comment, and your questions help me create content that actually addresses what readers want to know.
Healthcare practitioners: Have experience with electromagnetic pelvic floor therapy? We'd love to hear about your clinical observations. Email [email protected] to share your insights.
If you found this helpful, consider sharing it with someone who might benefit from understanding the evidence behind electromagnetic therapy for pelvic floor disorders.
Disclaimer: This article is for educational purposes only and should not be considered medical advice. If you have pelvic floor concerns, consult with a qualified healthcare provider—ideally a urogynecologist or pelvic floor physical therapist—who can provide personalized assessment and treatment recommendations.